How Registries Gain Momentum and Achieve Lasting Value

Here at ArborMetrix, we’re focused on creating and delivering powerful product roadmaps that align with the industry and the needs of our clients and partners. These roadmaps help prioritize work, set expectations, and point us ever forward, toward our long-term vision.
But, roadmaps aren’t simply our own internal tools. We often provide roadmaps to our customers for their clinical registries. These plans outline how to take their data and software assets to the next levels for their populations. To be effective long term, your registry must continually evolve to address the growing needs of your clinician and patient populations.
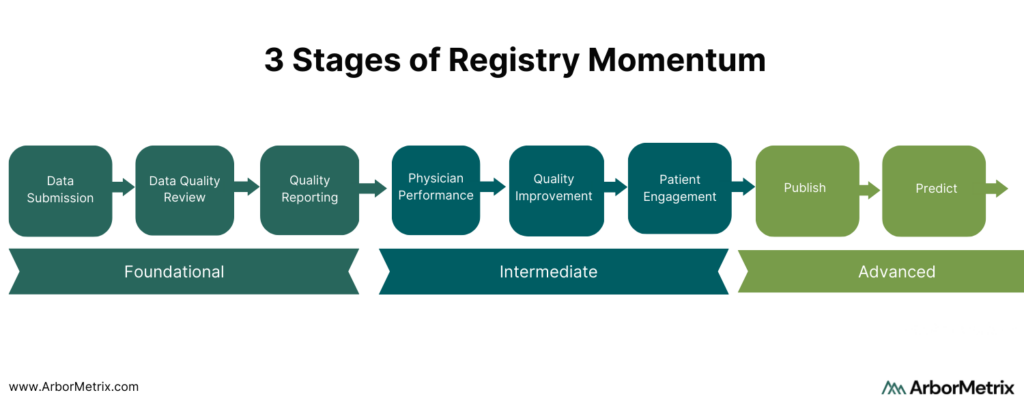
Clinical registries exist on a scale of momentum that spans three stages:
- Foundational
- Intermediate
- Advanced
We guide our registry partners through each stage and set a strategic plan to help them progress to their ultimate goals.
 Foundational Registry Momentum: Data Submission, Data Quality Review, Standard Reporting
Foundational Registry Momentum: Data Submission, Data Quality Review, Standard Reporting
Foundational registry momentum is defined by the compelling business and market needs that drive a registry’s framework. Often the impetus is collecting data for regulatory or post-market reporting, with features that include:
- Collecting data through a variety of channels and formats.
- Ensuring data is high quality through a robust data dictionary and supporting validation logic.
The Foundation stage is important because it serves to get data in the registry and drives membership and participation from affiliated organizations and clinicians. Most new registries achieve these goals within the first six months of launch.
However, if your registry launched a few years ago and you are feeling like your momentum is “stuck” or “limited” by not progressing past the Foundational stage, you’re not alone. This is a common situation that you can remedy with the right approach and technology.
Intermediate Registry Momentum: Clinician Performance, Quality Improvement, Patient Engagement
The momentum of your registry is truly unleashed when it builds deeper engagement.
This begins when it is used to highlight and change behavior. Our registry product and services are purpose-built for deep analytics and actionable insights related to measurable clinician and device performance, quality improvement, and patient engagement.
- Clinicians and industry stakeholders engage when the registry can be used to highlight their performance relative to peers and within their health system or specialty.
- Quality improvement is realized when the registry can indicate areas where treatments and interventions can be improved, and where guideline adherence is tracked and analyzed for impact.
- Patients engage when they are given the opportunity to safely share their health and quality of life related to diagnoses, treatments, and interventions, and know that data can be used in shared decision making.
Most of our clients spend a significant portion of their registry’s lifecycle building and growing these intermediate assets. This starts with our goals-oriented implementation process. These features can propel the momentum into new and relevant measurement areas and reporting domains that keep a registry fresh and engaging over time.
Advanced Registry Momentum: Publish and Predict
Finally, let’s talk about the hallmark of registry success: The ability to use it as a platform to publish research and clinical practice guidelines, and to predict outcomes. Advanced registries also expand their scope of participation and achieve sustainability through data commercialization.
Here’s how they reach this level. Registries arm us with trusted insights on clinician and device performance and quality improvement in care delivery. They also inform the patient experience through patient-reported outcomes. Registry owners and stewards share this knowledge and insights with the broader community to extend its impact.
Clinical Research and Practice Guidelines
Our customers have published a rich portfolio of registry-based research. Importantly, we help them achieve rapid-cycle research. On average, our customers publish their first peer-reviewed publication using registry data within a year of launch.
This is not just within scientific and medical journals, but also with the creation and publication of new clinical practice guidelines. The rigorous scientific process that we apply to registry data makes it ideal for evaluating the standards of care and long-term outcomes that impact patients.
Predictive Analytics and Outcomes Calculators
Predictive analytics is when data science principles are applied to model and forecast outcomes and risks at the point of care. This allows clinicals to make treatment decisions with better insight and, ultimately, avoid complications and negative outcomes.
The most advanced registries we support utilize outcomes calculators. These are built on complex data and models that combine foundational data assets with longitudinal patient data. Outcomes calculators provide powerful tools for shared decision-making between providers and patients and provide long-term registry value.
Predictive Analytics Registry Example
One example of an advanced registry using predictive calculators is the Michigan Bariatric Surgery Collaborative (MBSC). MBSC aims to advance the science and practice of bariatric surgery. Registry data is used to feed the MBSC Predictive Outcomes Calculator, which is publicly available for clinicians to use to predict a patient’s weight loss, comorbidity resolution, and complication rate after bariatric surgery.
Specifically, the tool:
- Predicts weight loss at years 1, 2, and 3 for five different procedures using patient information on demographics, comorbidities, and risk factors.
- Predicts the likelihood of resolving weight-related comorbidities.
- Predicts the likelihood of minor and major complications.
Notably, the predicted rates for weight loss, comorbidity resolution and potential complications are patient-specific, using risk-adjusted, real-world outcome data from similar patients.
These tools and other quality improvement initiatives helped MBSC and its members decrease rates of VTE by 43% and decrease post-surgical death rates by 67%.
Achieve Lasting Value with Your Registry
It’s important to remember that registry momentum happens over varying spans of time.
Some registries have been around for many years, and their momentum has been focused on providing foundational value to its members. Other registries are only getting started and are already looking at how they can propel their programs by quickly predicting outcomes and publishing results.
Whatever stage in which your registry exists, we have both the vision and the delivery model to help you build momentum and achieve lasting value.
Designing Healthcare Analytics to Engage Clinicians

Healthcare analytics software enables the acquisition, validation, transformation, and visualization of robust data sets. Organizations use healthcare analytics for a wide variety of purposes, including:
- The business of healthcare that analyzes financial trends and access to services.
- The delivery of healthcare aimed at driving improvements to the quality of care and care providers.
- The monitoring of healthcare treatments like devices and pharmaceutical interventions.
While the use cases are incredibly diverse, they all share a few common requirements:
- A dedication to the strict adherence to standards that keep your data safe and secure.
- A streamlined process for collecting and blending disparate data sources into a unified whole.
- A focus on improving access and outcomes for the most important stakeholder – the patient.
In order to achieve these aims, healthcare data must be engaging and interactive to support key decisions. This is especially true for clinician users.
User engagement is a key indicator to help organizations understand how decision makers like clinicians are using healthcare data and applications. User engagement metrics tell us:
- The degree to which data-driven decision making is prevalent in an organization’s culture.
- The degree to which the healthcare analytics application facilitates simple and intuitive data exploration.
At ArborMetrix, we see it as our responsibility to facilitate delightful and engaging user experiences and ultimately to inspire and support a culture of data-driven decision making in healthcare.
User-Centered Design in Healthcare Analytics
When designing healthcare analytics software to drive clinician and end-user engagement, it is crucial to understand the value proposition for key user personas. These personas represent the types of users and stakeholders who will be interacting with the product.
We leverage user-centered design principles to define personas and engage in best-practice research methods like focus groups, user observation sessions, and surveys.
Every persona has high-value needs, and we focus on designing easy and intuitive user experiences to facilitate those needs. Some examples of personas for clinical registries include quality officers, administrators, clinicians, researchers, patients and caregivers.
We tailor our user interface and workflows to align with the needs of our users. We want to ensure that they have easy access to the information and tools that matter the most to them.
Designing Healthcare Analytics Tools for Clinician Engagement
Here are a few examples of high-value opportunities for engaging clinical personas:
- Easing the burden of regulatory reporting requirements.
- Enabling meaningful benchmarks based on timely data.
- Providing quick access to relevant measures with robust filtering for custom patient cohort comparisons.
For users tasked with providing data, we aim to make data acquisition seamless by utilizing electronic connections whenever possible. When manual data entry is necessary, product capabilities for intuitive smart forms with validation logic that are attune with user workflows are critical. This is to ensure high-quality data capture with minimal effort.
It is important to capitalize on the momentum from an initial rollout of new software and plan a product roadmap to maintain engagement with new high-value capabilities and insights. Planning for growth can include expanding the scope of measures available, growing the library of reports, adding support for new personas, and releasing new product features that align with high-priority user needs.
Healthcare analytics software, purpose-designed for your users, can help you go beyond understanding how you’re performing to exploring why. That’s what inspires data-driven action and measurable improvement.

